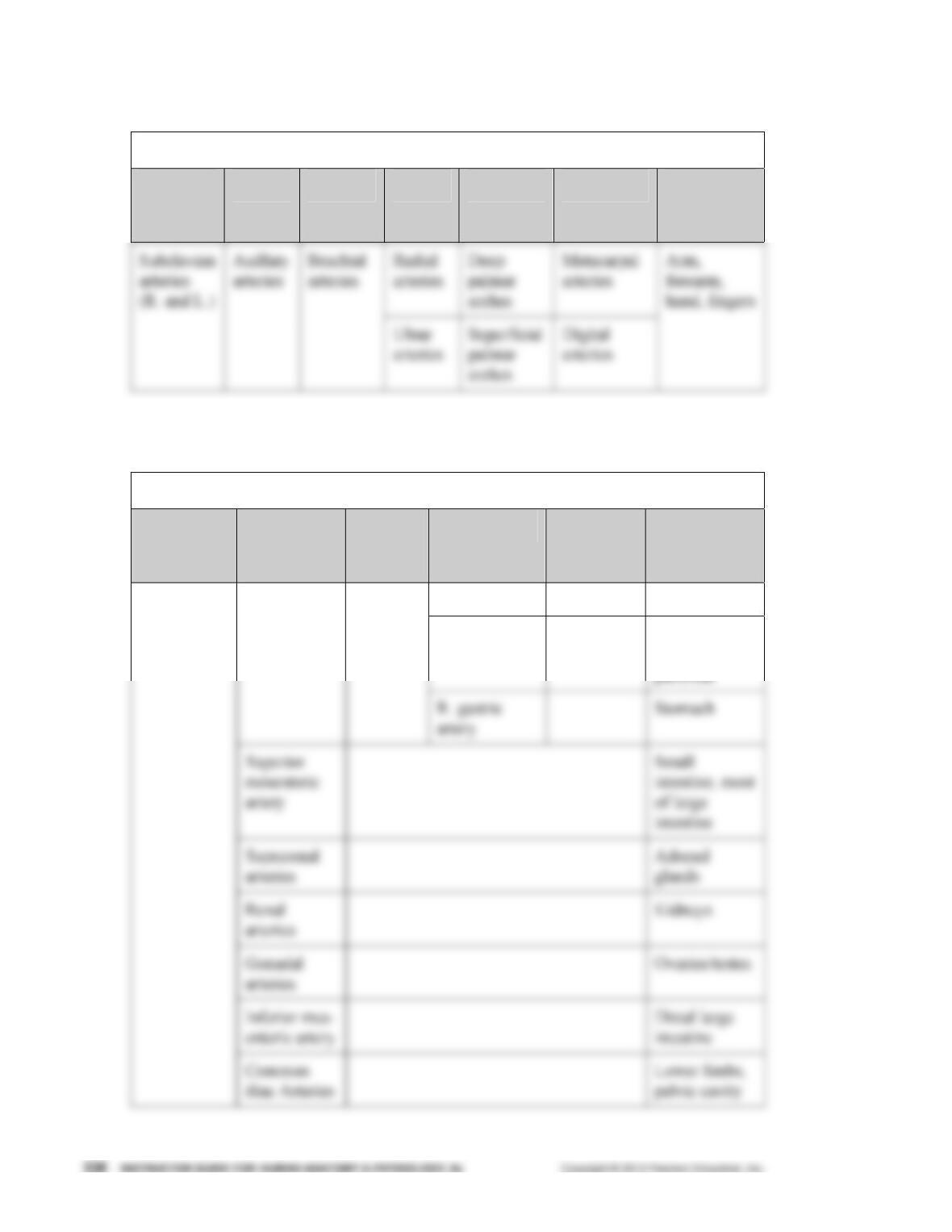
B. Capillary beds are microcirculatory networks consisting of a vascular shunt and true
capillaries, which function as the exchange vessels (p. 698; Fig. 19.4).
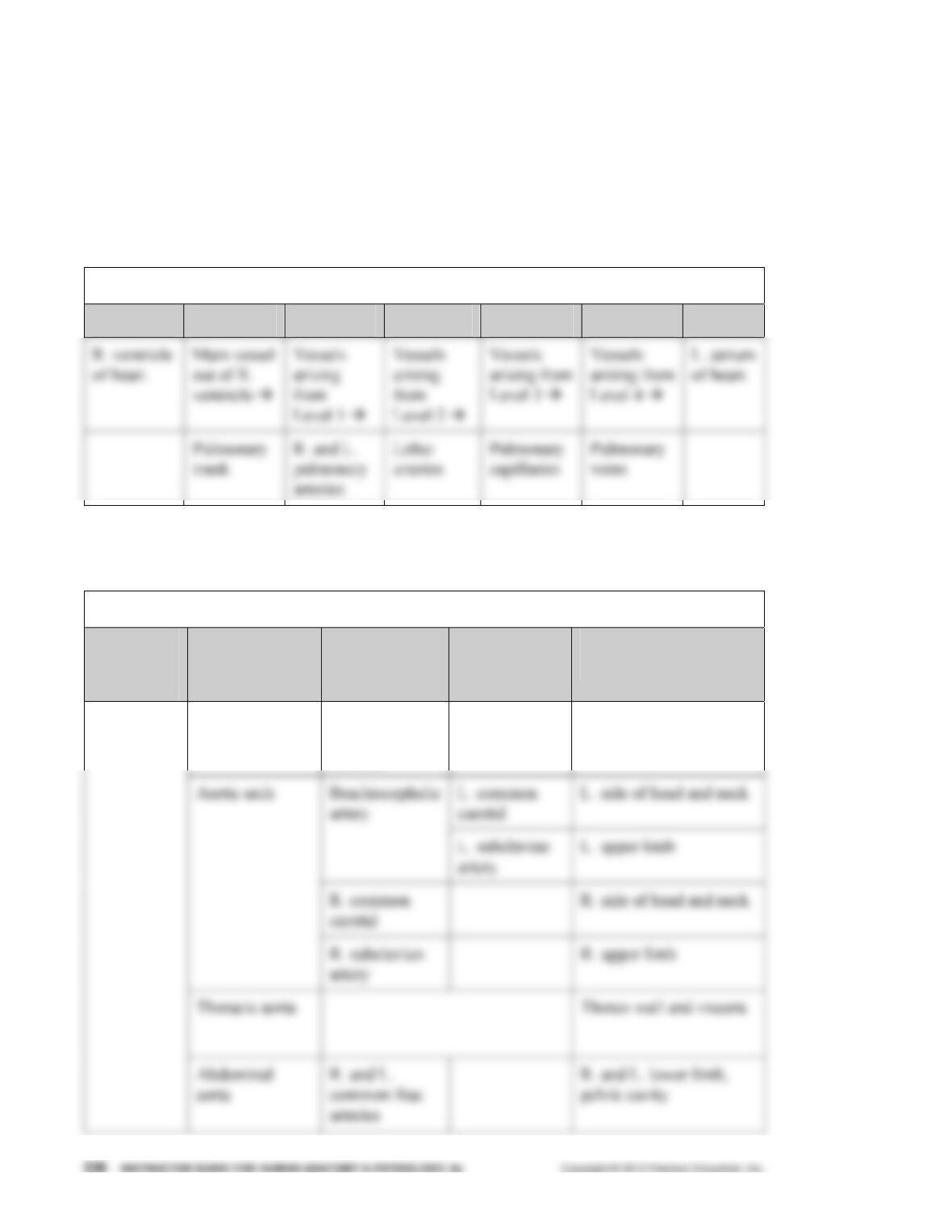
IV. Venous System (pp. 698–699; Fig. 19.5; Table 19.1)
A. Venules are formed where capillaries converge and allow fluid and white blood cells to
move easily between the blood and tissues (p. 698; Table 19.1).
Part 2: Physiology of Circulation (pp. 701–720; Figs. 19.6–19.18;
Table 19.2)
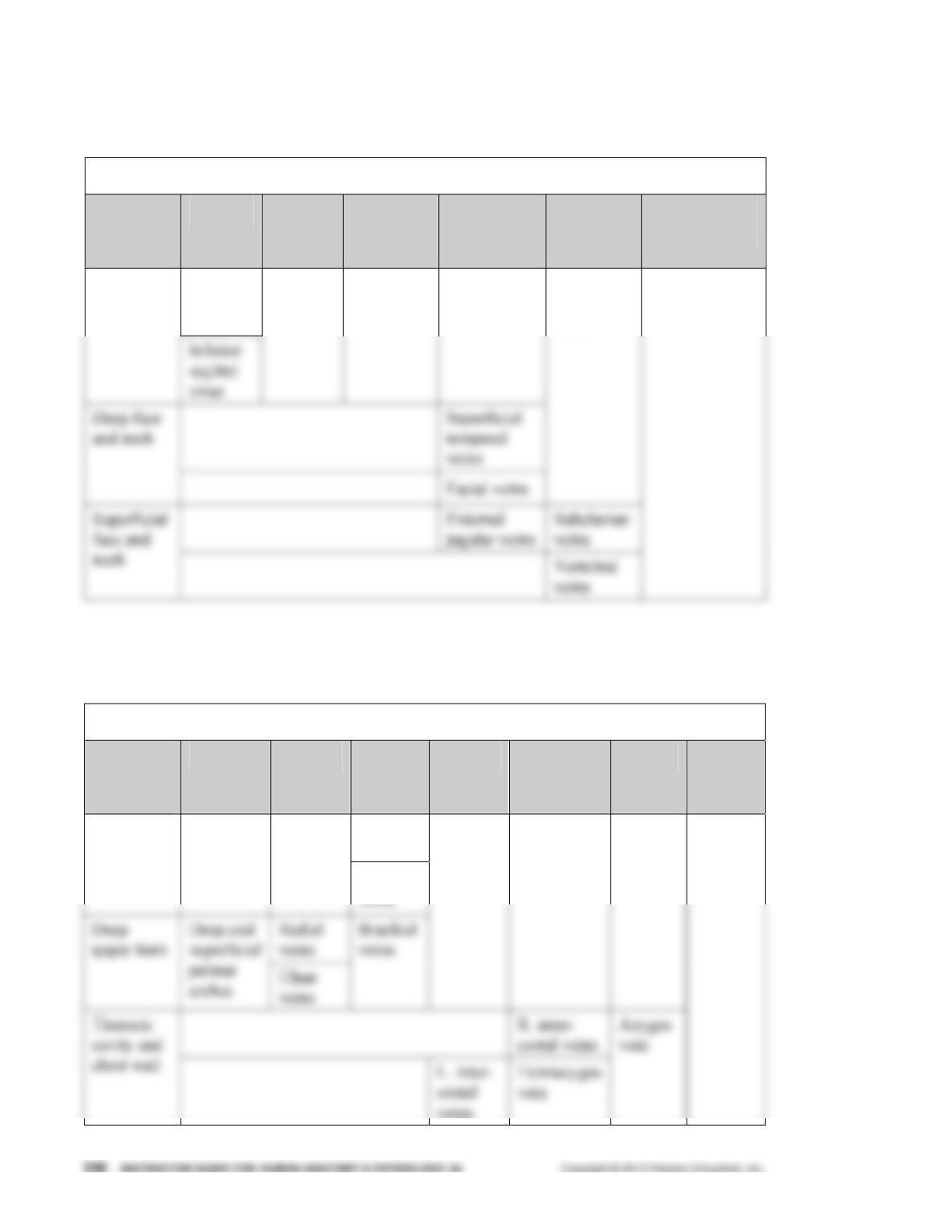
VI. Introduction to Blood Flow, Blood Pressure, and Resistance (pp. 701–702)
A. Blood flow is the volume of blood flowing through a vessel, organ, or the entire circula-
tion in a given period and may be expressed as ml/min (p. 701).
D. Relationship Between Flow, Pressure, and Resistance (p. 702)
1. If blood pressure increases, blood flow increases; if peripheral resistance increases,
blood flow decreases.
2. Peripheral resistance is the most important factor influencing local blood flow,
because vasoconstriction or vasodilation can dramatically alter local blood flow, while
systemic blood pressure remains unchanged.
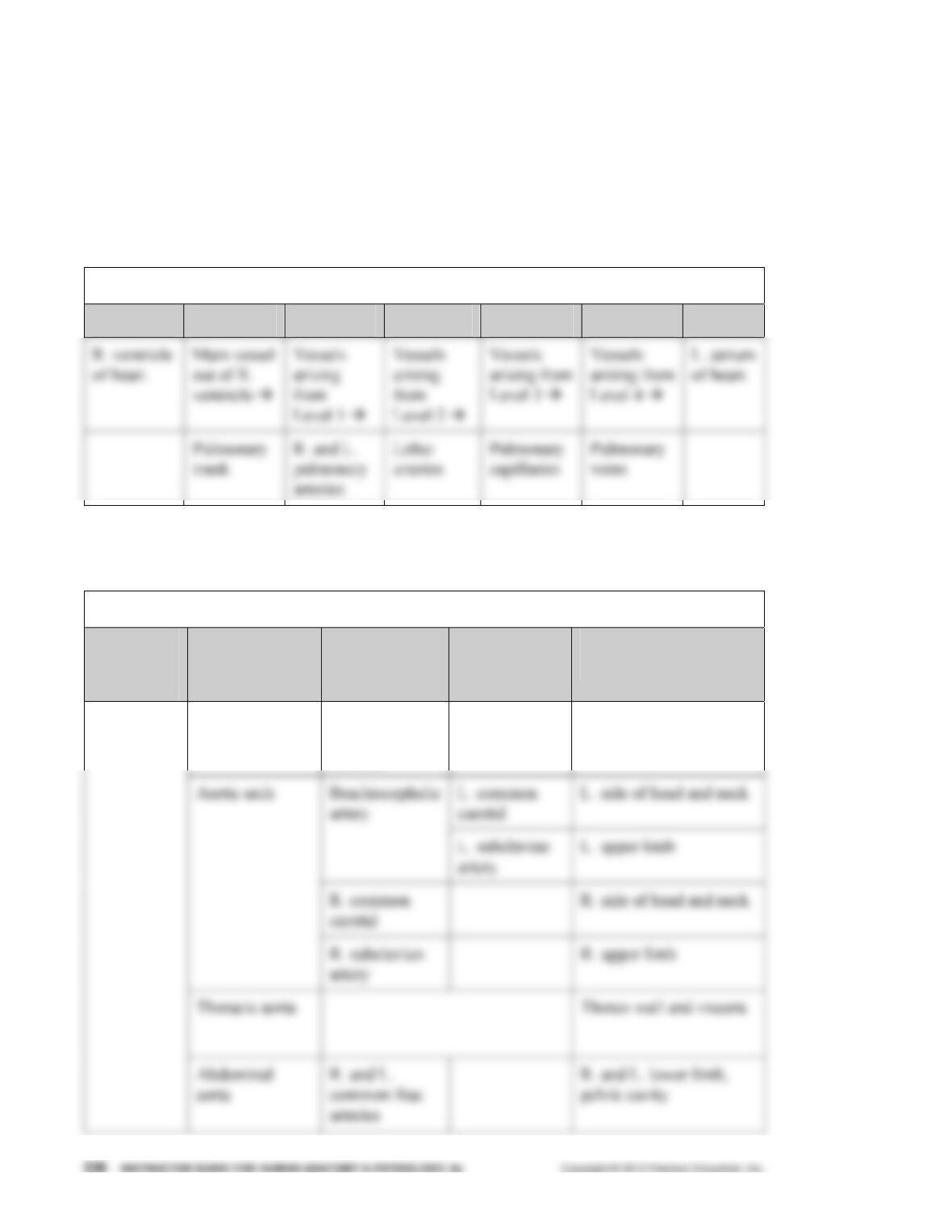
VII. Systemic Blood Pressure (pp. 702–704; Figs. 19.6–19.7)
A. The pumping action of the heart generates blood flow; pressure results when blood flow
is opposed by resistance (p. 702).
1. When the left ventricle contracts, blood is forced into the aorta, producing a peak in
pressure called systolic pressure (120 mm Hg).
2. Diastolic pressure occurs when blood is prevented from flowing back into the ventri-
cles by the closed semilunar valve and the aorta recoils (70–80 mm Hg).