Moghaddam A et al.
Shafa Ortho J. In Press( InPress):e4546
2
3.2. Risk Factors
Besides the type of fracture and the soft tissue damage,
there are other risk factors for the development of non-
unions (19). Smoking increases the risk of delayed heal-
ing or non-unions (5, 20). In addition, advanced age has a
negative effect on physiological fracture healing (21, 22).
Other factors such as diabetes mellitus, the use of non-
steroidal anti-inflammatory drugs (NSAIDs) and previous
fractures of the same extremity also have negative effects
(23, 24). In the risk score according to Moghaddam et al.
all of these risk factors have their relative importance for
measuring the individual risk of a patient for developing
a non-union (5) (Table 1).
3.3. Diagnosis
The diagnosis begins with extensive history taking and
includes the individual risk profile of the patient, taking
into account previous illnesses and medications as well
as all previous conservative and operative treatments.
History of previous infections should be taken into ac-
count as well as the analysis of previous clinical and ra-
diological findings. Blood circulation and soft tissue at
the site of injury should also be evaluated.
Clinical indications of non-union include pain on weight
bearing, limitations to the mobility of an extremity, or in-
stability. In addition, there are clinical signs of infection to
be aware of, such as redness, swelling and warmth or de-
velopment of a fistula. One should especially look out for
local, systemic or anamnestic signs of osteitis.
Conventional radiological imaging of the affected ex-
tremity in two levels with inclusion of joints is standard
for diagnosing faulty positioning or instability. One
should note that defects cannot be completely observed
with native X-rays due to summation and covering. An
additional computed tomography (CT) can be used to
evaluate whether there is partial or entire bridging of the
defect gap. In addition, a contrast magnetic resonance
imaging (MRI) can be used to evaluate vascularization of
the bone and separate vital and non-vital areas (25) (A CT
scan is considered the gold standard for evaluating non-
unions and providing information for treatment).
3.4. Classification
According to the current definition from European society
of tissue regeneration in orthopedics and traumatology (ES-
TROT), a non-union is a fracture that does not heal without
further intervention, independent of the length of treatment.
Non-unions are classically divided into four types: hy-
pertrophic due to mechanical causes, atrophic due to
biological causes, defect, and infection non-unions.
Hypertrophic non-unions develop due to insuffcient
mechanical stability and can lead to formation of a callus
in the area of fracture. Bone consolidation does not occur.
If therapy is delayed, atrophic non-unions can develop
(26). Atrophic non-unions often involve reduced vascu-
larity of the defect gap and surrounding bone, which can
lead to atrophy of the fracture ends. Defect non-unions
usually occur due to high-speed trauma and higher grade
open fractures, which can cause loss of bone through nu-
merous fragments. Furthermore, infected non-unions
develop primarily in open fractures after traumas in
which germs can get into the wound.
Besides the purely morphological classification, there is
a new classification system according to the non-union
scoring system (NUSS) which incorporates bone quality,
soft tissue damage, and the individual patient risk (e.g.
smoking) into a score (27). From this NUSS-score, there
are therapy considerations that can be adapted to the pa-
tient (28-30). The higher the score, the more specialized
and custom the therapy concept must be to offer the pos-
sibility of consolidation (Table 2).
3.5. Therapy
The goal of non-union therapy is the consolidation of bone
defects with correction of the axis and leg length as well as
reaching weight bearing stability. A suffcient tissue covering
as well as removal of the infection are the basic prerequisites.
Independent of the type of non-union and localiza-
tion, therapy can differ in conservative and operative ap-
proaches.
3.5.1. Conservative
Conservative approaches are especially useful in the early
phase of non-union treatment and require suffcient me-
chanical stability as well as bone regeneration potential.
The newest methods in conservative treatment in delayed
fracture healing of the lower extremity are consequential
weight bearing until full weight bearing can be mustered.
The most common methods of conservative treatment in
delayed fracture healing in the area of the lower extremity
are consequential weight bearing to full weight bearing.
Additionally, fractures are treated with daily lower ener-
gy ultrasound (a possibility of conservative therapy is the
application of low energy ultrasound to the defect gap),
over a defined interval of three to six months.
The deciding criteria for successful treatment with low
energy ultrasound are suffcient stability as well as a de-
fect gap of under 10 mm, free of infection in the previous
history, start of therapy in less than five months after the
fracture, and a NUSS-score less than 35 (31).
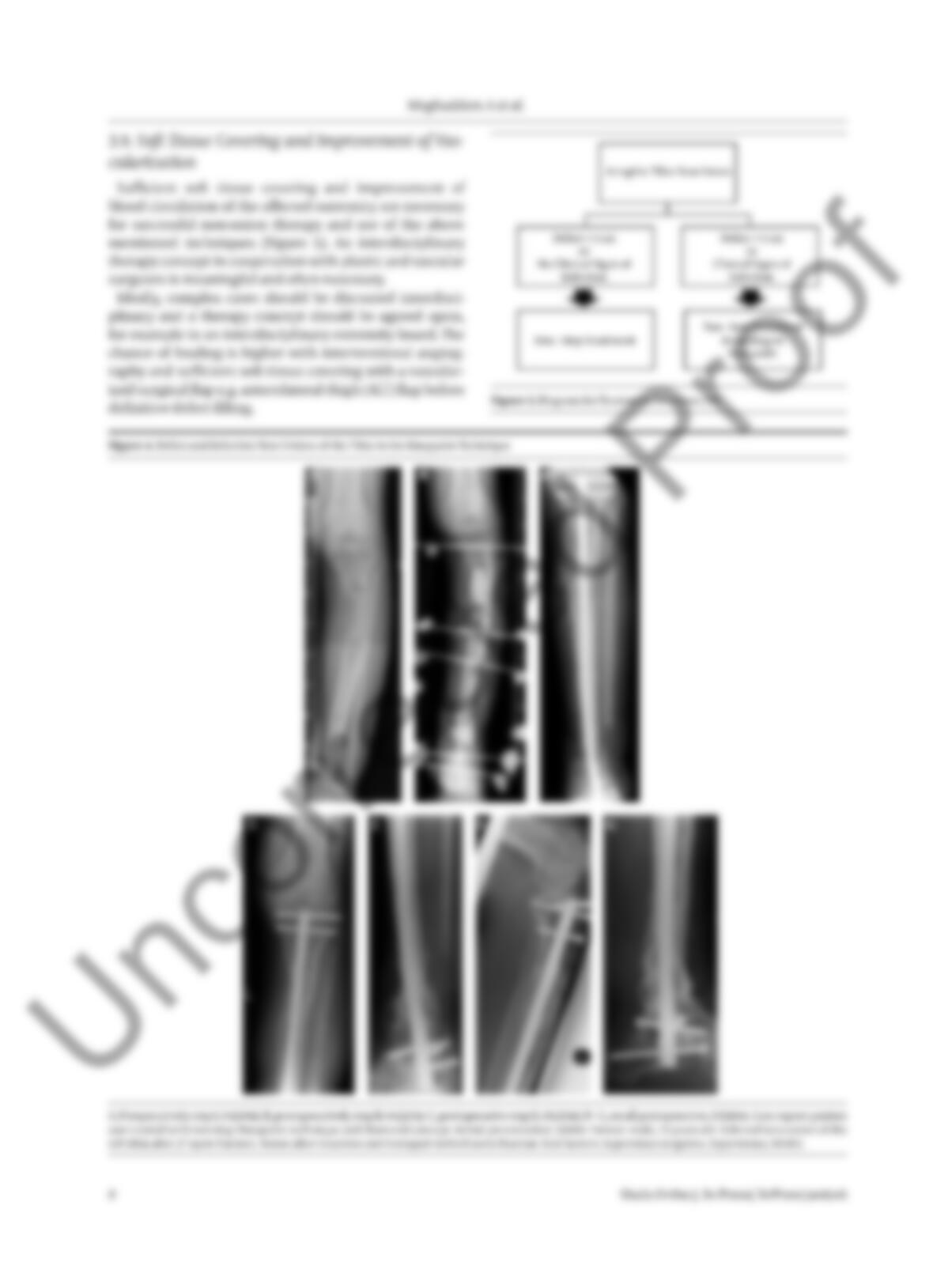
3.5.2. Operative Treatment Diamond Concept
The multi-factorial causes of delayed fracture healing
make an individual patient’s specific therapy noteworthy.
In this way, the so-called diamond concept (Figure 1) has
become evermore established (3, 32). Therapy consists of
an optimized combination of biological and biomechani-
cal factors (29, 33-38) (The diamond concept has five differ-
ent factors that must be analyzed for therapy) (39).
Non-unions are analyzed according to the following criteria:
- Biomechanical stability; example: through angle sta-
ble implants, dynamized medulla nailing.